Bacteria, biofilms, antibiotic resistance, and why some infections just keep coming back…..
by Siobhanne Thompson, (BNHM)
Biofilms are made by bacteria and occur almost as frequently as infections themselves. Biofilms form the plaque on your pearly whites, and the slime on your kitchen cloth. Not all biofilms are bad though… your kombucha SCOBY is a biofilm too!
 Biofilms protect and nourish bacteria
Biofilms protect and nourish bacteriaResearch demonstrates that pathogenic biofilms are able to withstand high doses of antibiotics and therefore allow chronic infections to develop and persist in the human body. Biofilms are well understood in medical settings as they tend to form around tubes inserted into the human body and increase the infection risk exponentially. Biofilms are also implicated in chronic conditions such as bacterial vaginosis, otitis media (ear infections), chronic sinusitis, and small intestinal bacterial overgrowth (SIBO).
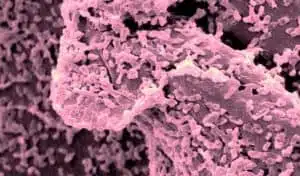
A bacterial biofilm is a thick, gummy, polysaccharide-rich matrix. It is created by undesirable bacteria that adhere to our mucosal surfaces when they are presented with opportunities such as low immune function and depletion of beneficial bacteria. Growing populations of bacteria species use a phenomenon known as quorum sensing to cohabitate, communicate, adapt and survive. Once established, the biofilm is a formidable adversary. It cannot be easily washed away, targeted by the immune system, nor easily eradicated with antibiotic treatment.
Bacteria, Biofilms & Bacterial Vaginosis
Biofilms are produced by bacteria and are known to be associated with bacterial vaginosis.
Bacterial vaginosis (BV) is the most common cause of abnormal vaginal discharge in women of reproductive age. It is a debilitating condition that can have an negative impact on energy levels, self-esteem, and intimate relationships.
Bacterial vaginosis is characterised by low vaginal acidity (pH>4.5), depletion of Lactobacillus species, and – although 50% of women with BV may not have symptoms – a fishy-smelling, greyish vaginal discharge is common. The depletion of Lactobacillus species allows other bacteria, mainly Gardnerella vaginalis, to set up shop in the vagina and get started on the formation of a thick, resilient, sticky biofilm.
The specific cause of BV is still unclear. What we do know is that factors such as cigarette smoking, intrauterine contraceptive devices (IUDs), and stress can all increase the risk of developing BV. If left untreated, BV can lead to more serious health consequence such as pelvic inflammatory disease, pre-term birth and pregnancy loss, and increased susceptibility to sexually transmitted infections.
Metronidazole is the standard treatment for BV, which does sometimes work. However, research demonstrates that bacterial vaginosis is a repeat offender, often reoccurring within weeks of antibiotic treatment.
What your naturopath can do…
Naturopathic treatment aims to disrupt and remove the biofilm. Treatment will also focus on up-regulating the body’s natural defences by restoring optimal pH levels and improving immune function. Your naturopath will also aim to improve your nutrition, and recommend beneficial strains of bacteria chosen specifically for their ability to maintain a healthy vaginal environment.
Bacteria, Biofilms & Chronic Sinusitis
Sinusitis is an infection of the upper respiratory system (airways) that can involve one or more sinuses. When it lasts for more than 12 weeks it’s considered chronic.
Increasing amounts of evidence have confirmed the presence of biofilm in patients with chronic sinusitis. It is the most likely cause of recurrent infection, which is known to persist despite surgical intervention and long-term antibiotic treatment. The prolonged inflammation associated with chronic sinusitis is likely to have caused damage to the lining of the airways, reducing cilia (the fine hairs that help to trap and remove dust, pollens, microbes and so on), and making it even harder for the body to get rid of mucous. Problems such as facial pressure, nasal congestion, and airway obstruction can all affect sleep and energy levels. This can limit the enjoyment of a number of activities, and greatly reduce the potential for optimal quality of life.
While the biofilm may not have been the initial cause of sinusitis, it is most probably the reason it is not responding to antibiotic treatment.
What your naturopath can do…
Whilst the bacteria within the biofilm are able to tolerate and continue survival after antibiotic treatment, they become susceptible when the biofilm is disrupted. Naturopathic treatment aims to disrupt and remove the biofilm. Treatment will also focus on addressing inflammation, healing the upper respiratory mucosa and up-regulating the immune system.











