
© 2023 House of Health. All rights reserved.
Web Design by Netbloom
Web Design by Netbloom

Polycystic Ovary Syndrome (PCOS) is an endocrine (hormone) and metabolic disorder that affects between 6 and 20% of women. It impacts many hormones, including androgens (such as testosterone), insulin, oestrogen, prolactin, follicle stimulating hormone (FSH) and luteinising hormone (LH). [1,2,3,4]
The signs and symptoms of PCOS are primarily related to elevated levels of male hormones (androgens), and not ovulating (called anovulation). [5]
A common symptom in PCOS is irregular menstrual cycles, most often longer than 35 days, or even skipping a period completely for one or more months. Women with PCOS may have challenges conceiving and experience recurrent miscarriages. Other common symptoms are excess hair in unwanted places such as the chin, the lower belly or insides of the thighs (this is known as hirsutism), acne (typically “male-pattern”), loss of head hair and carrying excess weight. [1,6,7]
No single cause of PCOS has been identified, and several risk factors have been identified. These are outlined below.
1. Insulin Resistance
Insulin resistance is generally accepted as the most common driver of PCOS. This occurs when sensitivity to insulin has decreased, which negatively impacts blood sugar levels. In the early stages of insulin resistance, the blood sugar may be normal, but insulin levels are elevated. This can lead to weight gain, heart disease, osteoporosis and eventually diabetes. It can also cause high male hormones (androgens) when there is genetic susceptibility to PCOS (see below).
Too much insulin can also interfere with ovulation. Insulin also negatively impacts other hormones, such as luteinising hormone (LH) and sex hormone binding globulin (SHBG), which can also contribute to further increases in androgens.
Insulin resistance is caused primarily by carrying excess body fat and having a diet that is high in sugar and processed foods. Smoking, stress, alcohol, and gut dysbiosis (an unhealthy balance of bacteria in the gut) may also contribute to its development and/or progression.
Carrying excess weight around the abdomen is a typical sign of increased risk of insulin resistance, however it is also possible to be a healthy weight and still experience insulin resistance and PCOS [2,3]
2. The Oral Contraceptive Pill
Coming off the oral contraceptive pill (“the pill”) can cause symptoms that might mimic PCOS, however this is usually temporary. As the pill supresses ovulation, it can take time for normal ovulation cycles to resume. Certain types of the pill strongly suppress androgens, and coming off them can cause a surge in androgens that can take up to a year or two to come back down again. [2,6]
3. Inflammation
Inflammation disrupts hormone receptors and suppresses ovulation – both can contribute to PCOS. Inflammation can also stimulate the adrenal glands and ovaries to produce more androgens. Conversely, PCOS is itself an inflammatory condition, where there is long-term low release of pro-inflammatory factors. [2,8]
4. Having Polycystic Ovaries
The name of the condition (polycystic ovary syndrome describes) the numerous small cysts (fluid-filled sacs) that commonly form in the ovaries in women with PCOS. When identified on ultrasound, there are usually numerous follicular cysts about 2-6mm in diameter, which are seen on the peripheries of a classically enlarged ovary. These cysts make androgens.
It is important to be aware that some women with this disorder do not develop ovarian cysts, and up to 20% of women have cysts on their ovaries, without developing the disorder. This suggests that other factors are involved.
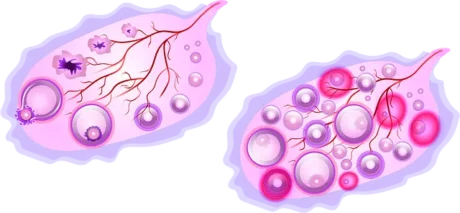
Diagram comparing the normal ovarian cycle on the left, with the process of development of multiple cysts due to halted development of follicles in PCOS on the right.
5. Genetic predisposition
About 40% of women with a family history of PCOS will have PCO, but may not develop PCOS.
Many of those who are affected often have both male and female relatives with type II diabetes, obesity, elevated blood triglycerides or high blood pressure. They may also have female relatives with infertility, hirsutism or menstrual problems.
In spite of these familial connections, no clear genetic link has been identified to date.
6. Ovarian dysfunction
This can lead altered hormones, such as low oestradiol and high ovarian androgens resulting in excess androgens (male hormones).
7. Excessive weight gain
As weight gain is the major risk factor for insulin resistance, this is considered an important modifiable risk factor. A high amount of adipose tissue leads to the conversion of androgens to oestrone.
8. Adrenal dysfunction
An important site for androgen production in women is the adrenal glands. Thus excessive production of androgens by the adrenals is a potential contributor to risk for polycystic ovary syndrome.
9. Certain medications.
Some medications are associated with PCO and hyperandrogenism. A common examples is the anti-epileptic medication valproate.
PCOS is a syndrome (essential a collection of symptoms), so diagnosis involves a full medical and menstrual history and assessing of symptoms, rather than a single, definitive test.
The condition is generally diagnosed when a woman meets two or more of the following three criteria:
For confirmation of the diagnosis, other reasons for high androgens (such as ovarian and adrenal gland tumours) need to be ruled out [17]. Monitoring blood sugars and cholesterol levels is also recommended. Your practitioner can also check fasting blood sugar with insulin to determine the impact that insulin resistance might be having.

It is not necessary to have polycystic ovaries for a diagnosis, and polycystic ovaries alone do not confirm diagnosis, as there are other situations when they can occur. Classification has moved away from emphasis on polycystic ovaries, and PCOS may eventually be renamed.
Some names that have been suggested are Metabolic Reproductive Syndrome (MRS) and Anovulatory Androgen Excess (AAE), as they better represent the condition. [2]
The gut microbiota refers to all the microorganisms within the digestive tract. It is so important that it may be considered an organ in its own right. The gut microbiota plays a number of key roles, not just in digestion but also metabolic health, immunity, regulation of the nervous system, drug and hormone metabolism and many others that we are continuing to learn more about through emerging research.[7]
Problems related to the gut microbiota can arise when there is a low number of beneficial microorganisms, a high level of harm-causing (or potentially harm-causing) microorganisms, or an overall low diversity of organisms (simply put, this means there is limited variety).[3]
Many studies have found connections between Polycystic Ovary Syndrome and the gut microbiota. Some of these include:
A medical approach aims to manage the symptoms. Just how will depend on the woman’s stage of life and the symptoms.
Examples of strategies for specific symptoms include:
None of these pharmaceutical options are without risk of adverse effects[18].
The single most important strategy for managing PCOS is losing excess body fat. This reduces the levels of male hormones (androgens) and improves insulin sensitivity. If a person is overweight, even a 5% reduction in body weight can significantly reduce the risk of developing type 2 diabetes and improving PCOS.
Exercise
Regular, moderate levels of exercise aids in sensitising the muscles to insulin. Going for a walk after eating a meal can help with blood sugar management.. Resistance training increases metabolism at rest.[2,3,6]
It is best if an exercise regimen is implemented under guidance, as those with increased androgens may develop male-type muscularisation fairly quickly.
Diet
Dietary modification and lifestyle change go together to make sustainable changes. Increasing fibre intake aids the gut microbiota, and can aid the excretion of hormones. Increasing the intake of foods high in magnesium (e.g., Brazil nuts, dark chocolate (80%+ cacao), brown rice, legumes, cashews, spinach, almonds, pumpkin and chia seeds) and zinc (e.g., oysters, beef, pork, cashews, sunflower, hemp and pumpkin seeds) can help improve insulin sensitivity, , reduce inflammation, promote ovulation and reduce androgens. Reduction in acne lesions may also be a result.[2,14,15]
Reducing the intake of sugars and refined carbohydrates, and increasing protein intake, especially at breakfast helps keep insulin levels low and provides sustained energy, which helps reduce the temptation to snack between meals.[2] Ultimately all are beneficial.
Dietary Supplements
Myo-inositol is a nutritional supplement which can help improve insulin sensitivity, decrease androgen levels and support regular ovulation.[2,13]
Pro and prebiotics
A probiotic is a living organism, while a prebiotic can be thought of as a food for those organisms. Both can improve microbiome diversity and insulin sensitivity, and help reduce LPS, inflammation and intestinal permeability.[9,13]
Herbal Medicine
Some herbal medicines can be helpful to reduce androgens, improve insulin sensitivity and support restoring a healthy gut microbiota. We recommend working with a qualified herbalist who can formulate a prescription specific to your needs.
Some women can completely reverse PCOS by making changes to their diet and lifestyle. Determining the levels of hormones is a crucial factor in planning those changes. Evaluation of insulin levels, via a standard laboratory test, determines the role of this hormone in managing your weight. Working with a health professional who understands your health goals, who can work with you to strategise a long-term solution is key to living successfully with this condition.
Showing all 2 results





Long before the advent of probiotic supplements, humans included fermented foods in the diet. In fact the earliest evidence we have, suggests
Book a Consultation with an Expert Here Contact Us Contact Us Agreement* I agree to the Privacy Policy.Subscription By sending this email,
House of Health Ltd
Due staff shortages, please use the website, phone or email to place your order. We will let you know when your items are ready for collection. Dismiss
Stay informed: Get expert tips, free advice, updates, recipes, and special offers delivered straight to your inbox.