Understanding Post-Infectious IBS
Post-infectious IBS is a condition where irritable bowel symptoms (IBS) like stomach pain, bloating, and diarrhoea start after you’ve had food poisoning. These symptoms can last for years after the infection itself is gone. In this scenario, one can pinpoint the time when the change in digestive function happened. But getting any acute tummy bug as a child also increases the risk of developing IBS later in life.
Why It Happens
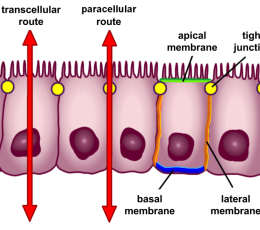
The reasons behind PI-IBS are complex and involve changes in how your gut moves and its sensitivity, increased gut permeability, meaning (often the wrong) things can pass through the gut lining more easily, and ongoing inflammation. This is likely due to an initial disruption caused by harmful bacteria, such as Campylobacter, E. coli, Giardia, and others, affecting your gut’s normal functions and causing chronic inflammation.
In New Zealand, outbreaks of water-borne gastro bugs are common, with recent newsworthy episodes in Kawerau in late 2019, and Havelock North in 2016, increasing the risk of IBS in these populations.
Crucially, these changes include significant shifts in your gut microbiota—the complex community of microorganisms living in your digestive tract. These microbes play a crucial role in maintaining gut health, aiding digestion, and regulating your immune system.
Gut Microbiota’s Role
The alteration in gut microbiota during and after the infection is particularly significant. Patients with PI-IBS can have quite an alteration in their microbiota composition compared to other people, impacting everything from gut motility to how the body processes emotions and manages inflammation.
Your gut microbiota influences gut motility, visceral hypersensitivity (and therefore pain), immune response, psychological function, sleep disturbances, serotonin, and bile acid metabolism, which are associated with digestive problems including IBS.
Maintaining a healthy gut microbiota is therefore essential not only for preventing PI-IBS but also for improving outcomes once it has developed.
COVID-19 and Your Gut
Interestingly, getting the COVID-19 virus can also impact the gut. The virus can bind to certain receptors in the gut, and has been found in the stool of many patients. The virus impacts gut cells and has been shown to alter gut microbiota, potentially triggering or worsening gastrointestinal symptoms.
Special Investigations
Small intestinal bacterial overgrowth (SIBO), is common in about a third of people with post-infectious malabsorption syndrome (aka “tropical sprue”) and about 20% of those with IBS-D. This is diagnosed with a hydrogen-methane breath test, which can help diagnose SIBO in patients with PI-IBS. Additional research has shown that testing for anti-cytolethal distending toxin B and anti-vinculin antibodies is effective in diagnosing not only IBS-D but also PI-IBS, particularly in patients with ongoing diarrhoea.
Managing and Preventing PI-IBS
The risk of developing PI-IBS can increase due to several factors including the severity of the initial illness, whether you’re a smoker, and even your psychological state, like stress or anxiety. Your baseline gut microbiota has a key part to play in how likely you are to get gastro, and how severely you get it.
Preventing PI-IBS involves more than just managing symptoms; it’s about enhancing your gut’s overall health and maintaining a robust gut ecosystem.
The mucosal immune system, which is crucial for maintaining the integrity of the intestinal barrier and controlling inflammation, plays a central role.
The gut microbiota, especially in early life, is vital in the maturation and regulation of this immune system. It helps ensure that inflammation is kept in check and that the body can tell the difference between harmless and harmful bacteria. This symbiotic relationship supports gut homeostasis, but when disturbed, can lead to a compromised mucosal barrier, abnormal immune responses, and increased risk of chronic inflammation and disease.
Therefore, promoting a healthy gut microbiota through diet, targeted interventions, specific prebiotics and probiotics, and supporting overall gut immune health is key to preventing infections and mitigating the development of conditions like PI-IBS.
With appropriate care, most people see a notable improvement in their symptoms and better overall quality of life as a result.
References
Thabane M, Marshall JK. Post-infectious irritable bowel syndrome. World J Gastroenterol. 2009 Aug 7;15(29)
Ghoshal UC. Postinfection Irritable Bowel Syndrome. Gut Liver. 2022 May 15;16(3)
Sanders DJ, et. al., The role of the microbiome in gastrointestinal inflammation. Biosci Rep. 2021 Jun 25;41(6)