What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune condition characterised by systemic chronic inflammation. It is caused by the immune system mistaking your tissues as foreigners and producing antibodies which attack those tissues. In RA this is the joints. If not controlled early this can lead to nodules, disfiguration of the joints, and other health complications 6
How Could the Gut Microbiome Lead to the Development of Rheumatoid arthritis?
The presence of concurrent digestive complaints in people with RA is common and with the known connection between the gut and the immune system, it is no wonder there is a link between dysbiosis and the development of autoimmune diseases, including RA.
The gut microbiome is important for homeostasis (balance) of the immune system and is an indicator of health 1. In those who are genetically susceptible, a combination of environmental factors can contribute to changes in the gut microbiota causing dysbiosis. This microbial imbalance increases the chance of developing chronic autoimmune disease through disruption of the immune system, likely due to the central role the gut and it’s microbial community has in immune function. 6
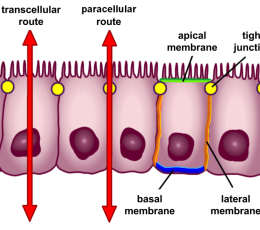
Two important influences on gut function and intestinal permeability are diet and the gut microbiome. 2 Together these factors can create a triad that either increases susceptibility, or protects against chronic diseases such as RA 2

The Bacteria – Rheumatoid Arthritis connection
A particular bacteria called Prevotella copri has been investigated for its role in the RA in multiple clinical trials. Results of these studies suggest that host genotype is associated with the microbiome before disease onset. 5
Significant differences in the population of gut bacteria exist in those with RA compared to healthy controls. People with RA tend to have higher levels of Prevotella copri and lower populations of of another major group of gut bacteria called Bacteroides. Pathogenic behaviour of Prevotella may be a causative factor in the development of RA, alongside other triggers in genetically susceptible people. 1
One theory is that Prevotella correlates with low levels of protective microbes. needed to regulate the immune system. Pathogenic bacteria, combined with diet, stress, and external factors such as environmental elements, can lead to mucosal inflammation. This inflammation may affect the body locally and systemically, eventually breaking immune tolerance through a mechanism such as molecular mimicry or direct facilitation of autoimmunity to self-antigens 2.
Other studies support the notion that RA is most likely the result of asymptomatic urinary tract infection with another bacteria, Proteus mirabilis. Still more evidence exists for relationships between Shigella and Yersinia (both are pathogenic), with increased gut permeability and activation of HLA-B27 self-antigen molecules 9.
SIBO and Autoimmunity
Other bacterial issues that may have a role in the disease process is small intestinal bacterial overgrowth, commonly referred to as SIBO. Simply put, that there is an excessive number of bacteria (either good or bad) in the small bowel. This can lead to significant digestive symptoms such as gas, abdominal bloating, constipation, and diarrhoea. Not only can this cause digestive discomfort, but it can also create a bit of mayhem in the gut increasing the risk of other health problems if not treated appropriately 7. You can read more about SIBO here.
Interestingly, a high number of participants with RA were found to also have SIBO. This study demonstrated that blood markers for rheumatoid arthritis (such as Rheumatoid factor titres) were significantly higher numbers of participants with RA had small intestinal bacterial overgrowth than those without. The possibility of bacterial overgrowth being associated with increasing or aggravating symptoms (or even may constitute as a contribution factor for development of RA is exciting. It opens a pathway for additional treatment options for those with RA who are SIBO-positive. Further research must be done on this subject to solidify this connection 3.
Managing and Treating Rheumatoid Arthritis
Discovering the link between gut health and the development of autoimmune conditions like RA, is exciting, but what does that mean for reducing the risk for those genetically susceptible to avoid the development of the disease? Better yet, what can be done to help those already suffering?
The confirmation of a gut-joint axis, as demonstrated in this research, highlights the importance of gut testing, to ensure the cause and treatment are appropriate for each case. The exact tests for you could include breath testing, stool microbiome, and/or intestinal permeability. Treatment options depend on the outcome, and could include:
- Dietary modifications
- Probiotics and/or prebiotics
- Herbal medicines and/or dietary supplementation
- Other recommendations to improve digestive function.
Topically applied, essential oils may also help alleviate the discomfort associated with rheumatoid arthritis. Read more here.
Dietary Modification
The microbiota composition of many people with RA undergoes changes as the disease progresses. A Mediterranean-style diet seems to influence the progression of RA, and may lower disease activity, and improve the outcome. 2
Not much research has happened when it comes to dietary intervention and RA, and currently the Mediterranean diet has the best evidence for reducing RA progression., However, dietary adjustments need to be carefully tailored to the individual to ensure the best results.

Probiotics to Restore Beneficial Bacteria
Some strains of probiotics have been shown to influence the immune system. This may by due to a reduction of specific molecules called pro-inflammatory cytokines and an increase of their counterparts, the anti-inflammatory cytokines associated with taking these probiotics.6 in clinical trials, specific probiotic strains from the Lactobacillus and Bifidobacterium families have been shown to reduce the symptoms of RA and while this strategy is an emerging therapy, it certainly offers promise as a low-risk treatment option1
Probiotics and/or Prebiotics to Reduce Pathogenic Bacteria
Addressing underlying bacterial imbalances could be a strategy for preventing those genetically predisposed to RA or reducing disease progression in those with the condition. A study on which people with RA were given antibiotics demonstrated reduction in the symptoms of RA. This further supports the gut-joint hypothesis, and the possible role of bacterial aggravators.
Following testing to determine the bacterial population, targeted treatment with botanical anti-bacterial agents may play a role in improving the condition. In another study, herbal alternatives were demonstrated to be as effective as rifaximin (a small-intestine-specific antibiotic) for reduction of bacterial overgrowths in SIBO 8.
The state of your gut plays a large role in overall health, with dysfunctions increasing the risk of chronic disease such as rheumatoid arthritis in those already susceptible.
Do you need help with rheumatoid arthritis or another auto-immune condition? Make an appointment with one of our holistic health experts using the booking button below.